Coronavirus transmission has been slowly, but steadily, on the rise in recent weeks — and though local public health officials say the most recently available data doesn’t yet indicate a surge akin to the spike in cases seen last winter, they are urging members of the public to take basic safety precautions ahead of the fall flu and back to school seasons.
The number of reported COVID-19 infections has nearly doubled in Los Angeles County over the past month, according to Department of Public Health director Barbara Ferrer, who held a press briefing on Thursday, Aug. 31, with virus-related hospitalizations following suit in recent weeks.
There were about 571 coronavirus cases reported this week, Ferrer said Thursday, up from about 264 reported in early August. Those numbers, though, are likely undercount since they don’t include the results from home tests.
“And while case numbers are relatively low compared to many other points this past year,” Ferrer said, “I also want to note that it’s a bit unfair to make those comparisons because there’s less reportable testing.”
Since the COVID-19 emergency ended at the federal, state, and local levels in the Spring, reliable testing results — like PCR or other lab tests — have dropped significantly, meaning that DPH has less virus data to work with, Ferrer said.
Hospitalizations, though, are a more reliable metric the health department uses to get an understanding of how widespread COVID-19 is, Ferrer said. Those have also doubled since the first week of August — with an increase to 521 coronavirus-related hospitalizations over the last week from just 245 on Aug. 2.
“(But) hospitalizations remain well below the numbers we saw during the 2022 summer and winter surges,” Ferrer said. “In fact, there were only four other periods during the entire pandemic where hospitalizations were lower than what we’re reporting this week.”
Another metric — the average weekly rate of coronavirus-related hospital admission per 100,000 people — which is used by the U.S. Centers for Disease Control to evaluate the virus’ risk, has also increased since July, the director added.
That number currently sits at 6.3 per 100,000 people, Ferrer said, meaning that the county still qualifies for the “low” risk category.
“If our COVID-19 hospital admission rate continues to increase at the same rate it has the past three weeks,” Ferrer said, “L.A. County could move to the ‘medium’ hospital admission level in about four weeks.”
Los Angeles County Dept. of Public Health Director Barbara Ferrer holds a COVID-19 briefing as cases rise in Los Angeles on Thursday, August 31, 2023. (Photo by Sarah Reingewirtz, Los Angeles Daily News/SCNG)
Since the CDC uses that specific metric to determine risk, if the county reaches the “medium” tier, their could be changes to DPH’s health orders in order to prevent further spread of the virus.
The COVID-19 death rate, though, hasn’t increased the same way. DPH is currently reporting about one death per week on average — but the department also tracks the percent of all deaths in the county that have been linked with COVID-19, Ferrer said.
About 2.5% of all deaths countywide were associated with COVID-19 according to DPH’s most recent data, Ferrer said — and increase from 1% two weeks ago. That number was about 5% during the winter surge and 7% during the summer surge last year, she said.
“It is possible that this could be an early indicator that we’re (maybe) going to see some increased numbers of deaths,” Ferrer said. “Yet, with only one week of data, it’s too early to determine if this is a trend.”
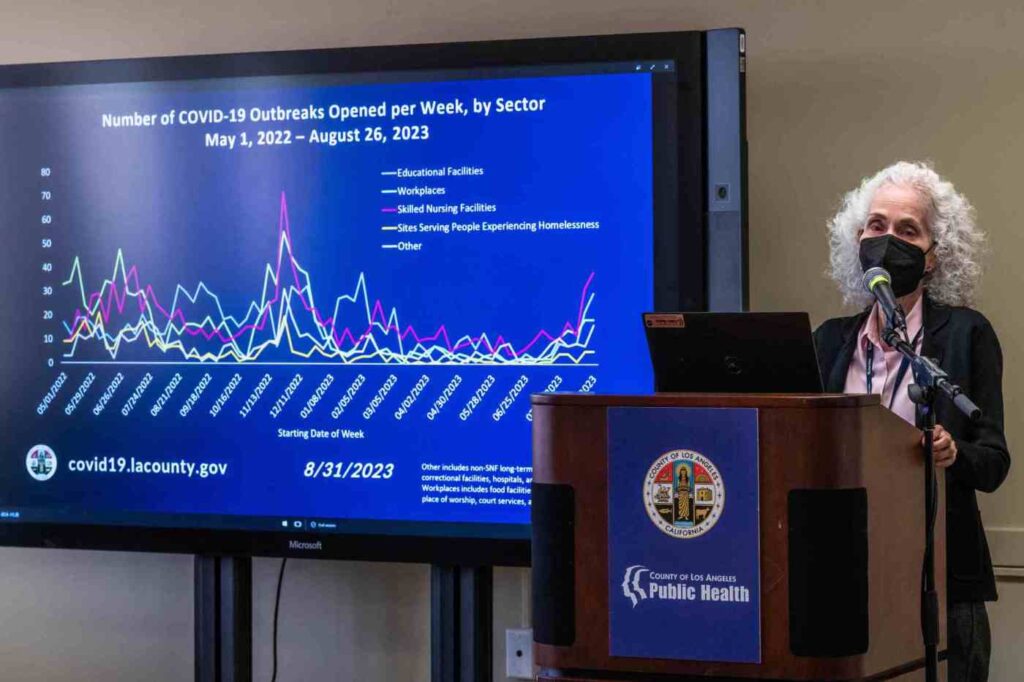
DPH also reported an increase of COVID-19 in its wastewater samples — which cover about 77% of all LA County residents — along with increased virus outbreaks in school, skilled nursing, and workplace facilities.
Virus strain EG.5 — a descendent of the omicron XBB strain — is currently the most dominant one in LA County, accounting for about 21% of DPH’s sequenced cases. This is significant, Ferrer said, as its the first time a single strain has made up more than 20% of the county’s cases since early July.
Coronavirus transmission has also increased in other major Southern California regions — including Orange County and Long Beach — though on a much smaller scale.
Long Beach, which has an independent health department, reported 217 cases over the last week, according to the city’s Department of Health and Human Services representative Jennifer Rice Epstein.
That’s slightly lower than the previous week’s metric of 269 for the week ending Aug. 24, Rice Epstein said. The week prior, ending Aug. 17, Long Beach’s case count totaled just 168.
There were nine hospitalizations in Long Beach over the past week, up from four two weeks ago, with no new deaths reported during that same time frame.
“We are not currently discussing changes (to our health orders), and we are following state guidance,” Rice Epstein said. “We continue to encourage common-sense measures like staying home when sick.”
The number of COVID-19 cases in Orange County has been steadily increasing since the beginning of May, county health officials said Thursday. Eleven deaths related to the virus have been reported in August.
About 17% of tests reported to county health officials are coming back positive, according to the county’s online database — but, again, the true number of infections is likely higher due to underreporting.
Although the number of hospitalized patients has slowly been increasing, Dr. Regina Chinsio-Kwong of OC Health Care Agency said Thursday, hospitalizations overall remain at low levels.
“Now is the time to for everyone to reassess and implement mitigation strategies — especially for those who are, or who work or live with, at-risk individuals,” Chinsio-Kwong said. “Improving indoor ventilation and the use of face masks can offer protection and reduce transmission.”
The CDC and World Health Organization, meanwhile, are also tracking a new coronavirus strain, BA.2.86, as as variant of “possible concern,” Ferrer said. It has 35 new mutations on the virus’ spike protein — roughly similar to the genetic differences seen in the original omicron variant.
That new viral lineage, though, only makes up about 1% of all COVID-19 cases nationwide, CDC director Many Cohen said during a separate Thursday press briefing, and no instances of it have been detected in California thus far.
Related Articles
Flying Food fined $1.2 million for lag in rehiring laid-off workers
Covid-19 has changed and so has our immunity. Here’s how to think about risk from the virus now
Updated COVID-19 vaccines are coming mid-September, officials say
‘Rock star’ California doctor lauded for COVID testing work pleads guilty to selling misbranded cosmetic drugs
Two years after catching COVID, patients still risk getting sick
“We are watching that closely,” Cohen said.
Nationally, meanwhile, COVID-19 transmission is also rising. There are currently about 15,000 people hospitalized for virus-related symptoms, according to CDC data for the week ending Aug. 19, up about 19% from the week prior.
This time last year, that number was about 38,000, according to Cohen.
“We’re at a level that’s less than half of what we saw just one year ago,” Cohen said. “Again, I think that is because we have more tools and more immunity than we’ve had before.”
About two percent of deaths nationwide from Aug. 20 to Aug. 26, meanwhile, were attributed to COVID-19, the CDC data show, a 17% increase from the week prior.
But despite those elevated metrics, Cohen said that the United States is more well-equipped than ever to prevent a significant surge in cases — largely because nearly 97% of Americans have some sort of immunity, whether by prior infection or inoculation.
There are also a few new tools in the arsenal to protect against Respiratory Syncytial Virus, Cohen said, which can cause serious illness in infants and older adults, and — alongside the flu and COVID-19 — contributed to an increased strain on hospitals during the winter surge last year.
The Food and Drug Administration, for example, approved the first-ever RSV vaccine for adults aged 60 and up in May.
In July, the FDA also approved a new drug to prevent the disease in babies and toddlers — and a month later, gave the OK for a new vaccine for pregnant people to prevent the disease from infecting their infants.
A newly updated COVID-19 vaccine booster, meanwhile, is expected to be available by the second week of September, Cohen said. It’s tailored to protect against severe illness from the variants that are dominant in both the U.S. and around the globe, and is currently under FDA review.
But once available, that added protection, along with common sense health measures like frequent handwashing and testing, will be crucial moving into the fall season — infamous for its proclivity to spread respiratory diseases — especially ahead of the Labor Day weekend and as kids continue their return to school.
Ferrer and the DPH are hoping there won’t be a major surge in COVID-19 transmission following the holiday weekend given the context that there wasn’t a massive spike in cases after the 4th of July, Ferrer said.
“There may be some increases associated with Labor Day, particularly because we also have a lot of children going back to school,” Ferrer said. “COVID-19 is still changing, and we can’t accurately predict what will happen in the fall — what we do know is how to be prepared to take appropriate safety precautions as needed to protect ourselves.”
Staff writer Destiny Torres contributed to this report.
